Palmar hoof pain refers to a syndrome of clinical signs, rather than a disease process itself. The term palmar is an anatomical reference meaning ‘rear facing’, such that palmar hoof pain means pain emanating from the rearward structures of the hoof in the forelimb. The term plantar references the rear facing structures in the hindlimb. Since the problem is more common in the forelimbs we will use the term palmar throughout this article.
In the hoof, those structures considered palmar include:
• Digital cushion
• Palmar processes of the pedal bone (the ‘wings’)
• Collateral cartilages• Surrounding soft tissue, including the sensitive heel bulbs
• The deep digital flexor tendon to the extent present within the hoof capsule
• Impar ligament
• Navicular bursa
• Navicular bone
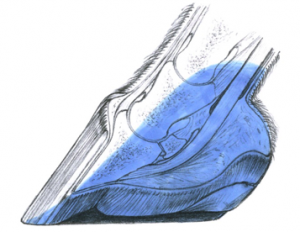
Typically, horses affected by palmar hoof pain will respond favourably to a palmar digital nerve block. As indicated by the diagram above, however, this localises the pain but does not identify the specific structures involved. Imaging is necessary to find the cause of the pain. There will be cases where no definite answer is reached, either because advanced imaging is unaffordable or it fails to find a cause. In these instances a horse is said to have palmar hoof pain syndrome.
The most common causes of palmar hoof pain are:
• Navicular disease
• Navicular bone fracture
• Insertional tendinopathy of the DDFT
• Sidebone (ossification of the collateral cartilages)
• Fracture of the palmar processes of the pedal bone
• Corns/Caudal heel pain (inflammation of the sensitive dermis of the heels)
Navicular Disease
Navicular disease (also referred to as navicular syndrome) is a chronic, progressive, dege
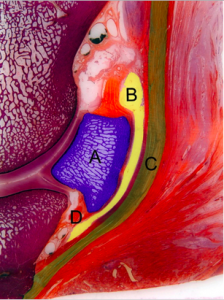
nerative disease of the navicular region. Forelimbs are most commonly affected, with the average age of onset between 7-12 years. The key area affected is the navicular bone, which is found between the palmar recess of the coffin joint and the deep digital flexor tendon. Other associated structures affected by navicular syndrome may include the navicular bursa, impar ligament and deep digital flexor tendon
A = navicular bone (blue)
B = navicular bursa (yellow)
C = deep digital flexor tendon (green)
D = impar ligament (orange)
Mechanisms of Disease
There are a few mechanisms thought to be driving the disease process.
• A repeated cycle of compression caused by the navicular bone being squeezed between the back of the short pastern bone and the DDFT. This is thought to cause inflammation and degeneration in the navicular bone and surrounding tissue.
• Increased tension in the ligaments supporting the navicular bone, in particular the impar ligament, can lead to focal inflammation
. Subsequent scarring and fibrosis can affect blood supply to the navicular bone.
• Altered perfusion caused by narrowing of the blood vessels leading to and from the navicular bone can cause pain and, over time, remodelling of the bone.
Conformation
Horses with steep pasterns and upright, boxy feet are particularly prone to navicular disease. The reduction in shock absorption due to decreased frog contact with the ground and relative inelasticity of the hoof capsule due to contracted heels, lead to an increase in concussion. The comparatively high body weight in relation to hoof size is another contributing factor in development of navicular disease. Quarter horses are over-represented as this conformation is relatively common in the breed.

Horses with long toe low heel conformation and a broken back hoof pastern axis are liable to experience increased t
ension within the DDFT, which in turn compresses the navicular bone. Degeneration of the digital cushion compounds the lack of support.
Clinical Signs
Affected horses typically present with a chronic progressive lameness of one or both forelimbs that is usually slow in onset, but may occasionally appear acutely after a change in how the horse is worked. It is commonly associated with a loss of performance, with temporary improvement after a period of rest or reshoeing. There may be more subtle signs of reduced performance prior to obvious lameness. Unwillingness to work, refusing jumps, less expression in paces, avoidance of hard, uneven ground. Intermittent mild lameness and an increased frequency of stumbling have also been reported. More advanced cases can show discomfort in the box, with a shifting of weight between forelimbs or alternately pointing forelimbs. Shoes may show excessive wear of the toe, as the horse may favour landing toe first.
Diagnosis
A thorough lameness examination will be carried out by the veterinarian. The following signs may be noted:
• A stilted, shuffling gait with a reduced ‘swing’
• Intermittent or continual light to moderate lameness
• A lameness that is increased on the inside leg when the horse is turned in a circle (especially on hard ground)
• Pain response to hyperextension of the palmar hoof region
• Pain response to flexion of the lower limb
• Pain response to application of hoof testers over the heel walls
• Pain response to application of pressure through the frog
Lameness is typically abolished via a palmar nerve block at mid-pastern level leading to the clinical diagnosis of palmar hoof pain. The disease is often present in both limbs, though one leg more affected than the other – hence switching lameness after a nerve block is not uncommon. At a later stage, a vet might place further nerve blocks (such as a coffin joint block or navicular bursa block) to exclude other diseases.
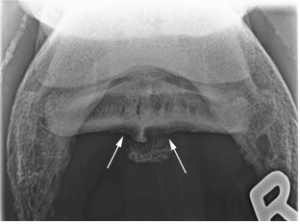
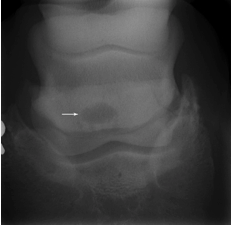
X-rays will be taken to assess the condition of the navicular bone. Classic signs of a diseased navicular bone include:
• Cystic lesions within the bone
• Defects in the flexor cortex
• Thickening of the flexor cortex, with loss of corticomedullary distinction
Note: The above changes are rarely seen in healthy horses and are highly suggestive of disease. The below changes are found in a significant number of normal horses and so are to be interpreted with caution. They are not considered pathological when encountered in isolation.
• Enlargement of the distal foramina (lollipop lesions)
• Bony spurs on the proximal and distal borders
More advanced imaging options such as scintigraphy, CT and MRI also have a role to play in complex cases.
Treatment
There is no curative treatment. Treatment is aimed at reducing inflammation and pressure within the hoof. There are a
wide range of medical treatments. Different horses respond differently to different treatments. Some horses require a combination of treatments for optimum relief.
Medical treatments of choice include oral analgesic and anti-inflammatory medication, corticosteroids injected into the coffin joint or navicular bursa, vasoactive drugs designed to improve blood flow, drugs affecting bone metabolism to delay bone loss.
In advanced cases, another possible method of pain relief is neurectomy of the lateral and medial palmar nerves. This treatment completely removes sensitivity in the palmar hoof. It is a symptomatic treatment which should only be undertaken to improve quality of life, it does nothing to prevent the disease from progressing. Horses that have undergone neurectomy should not be used for athletic acitivity, FEI regulations prevent them from being used in competitions.
Shockwave therapy has bee trialled with the aim of providing symptomatic relief, no controlled studies have yet confirmed the efficacy of this treatment.
The aim of therapeutic shoeing is to decrease the forces acting in the palmar hoof area. A balanced hoof with correct alignment of the hoof pastern axis should be established, so far as the hoof allows. A short shoeing interval is recommended. Reducing load on the frog will prevent direct pressure on the navicular region. Shortening the toe to ease breakover over the toe and the sides is important to relieve pressure on the palmar hoof. Applying a rolled or rocked toe and using shock absorbing materials can also be beneficial. Support in the palmar hoof region might also be established using an egg bar shoe. Egg bar shoes stop the heels from sinking into soft ground, preventing hyperextension of the coffin joint and overloading of the navicular. The bars of the shoes should not be applying direct pressure to the frog.
Prepared with reference to FEI Campus materials
